Finding relief from irritable bowel syndrome: Effective strategies for a better life
One in five people in Singapore suffer from it but the common condition is not easily understood
[SINGAPORE] Is irritable bowel syndrome (IBS) simply “caused by stress” and “not a real condition”?
For the one in five people in Singapore who suffer from it, it is very real indeed.
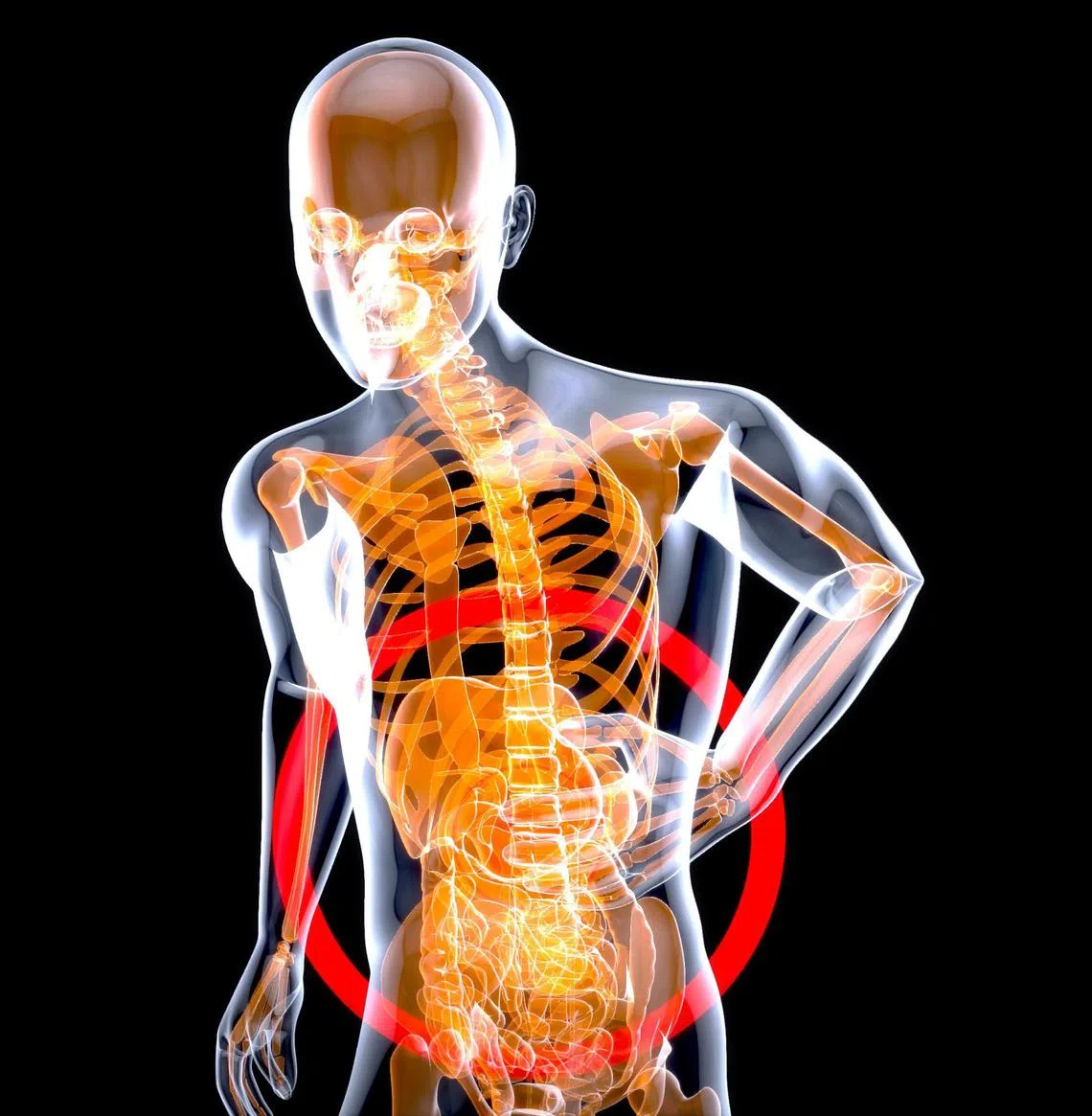
Characterised by chronic or recurrent abdominal discomfort or pain that is associated with changes in bowel habits such as diarrhoea, constipation or both, it is a common condition that is not easily understood.
The disorder tends to affect the large colon, although it does not cause structural damage or inflammation. “That’s why it’s a diagnosis of exclusion, meaning we would do scopes and scans to rule out organic causes such as inflammation or cancer, before we can say with more certainty that the symptoms are IBS-related,” says Dr Alexander Yip, head and consultant, division of gastroenterology and hepatology, department of medicine, Alexandra Hospital.
Some people who see him are very frustrated because they have been constantly waved off. “When patients are not guided through their condition, and they’re always in pain, it leads to erosion in confidence in their medical providers.”
With April being IBS awareness month, we explore the science behind the condition, unpack misconceptions about the disorder and find out what people should know about this complex gut-brain disorder with biological underpinnings.
What it is – and isn’t
IBS is a functional gastrointestinal (GI) disorder causing abdominal pain or discomfort – sometimes for years – and a sense of bloating or gaseousness. The diagnostic criteria stipulates that this recurrent abdominal pain occurs on average one day per week for the last three months. This is associated with patients alternating between suffering from diarrhoea and constipation, followed by a relief from pain or discomfort after emptying their bowels.

“The art of history taking is very important as patients are not going to tell us about these symptoms right away,” says Dr Yip. “So as doctors, we have to listen carefully and slowly tease these things out.”
As IBS does not cause inflammation – which is a key factor in colorectal cancer risk – it is therefore completely different from inflammatory bowel disease (IBD). IBD is “a much nastier thing”, as it causes swelling and inflammation in the digestive tract and can lead to cancer.
Gut-brain connection
There is no single known cause for IBS, which is thought to be a combination of visceral hypersensitivity – which is increased sensitivity to pain in the gut – psychological factors such as stress, anxiety and depression, gut microbiome imbalance and altered gut motility. It is a kind of “disrupted gut-brain communication”.
The gut-brain axis, explains Dr Yip, is like a two-way communication network between the GI tract and the central nervous system. “Sometimes, people say they have a gut feel and actually, your gastrointestinal tract does have a ‘brain’ and it’s called a peripheral enteric nervous system.”
Enteric refers to the intestines, and peripheral because it is not part of the central nervous system. This “highway” involves the nervous system, hormones, immunity and gut microbiome, all of which play crucial roles in maintaining digestive health and even emotional regulation and stress response.
“So that two-way, gut-brain communication is critical in maintaining balance. And when one tips over, maybe you won’t have any problems yet, but when you have a systemic failure, the dominoes start to fall and you begin to manifest IBS symptoms.”
Triggers
Sometimes, IBS is triggered by infections. Post-infectious IBS can happen after one gets food poisoning or even just a viral infection such as stomach flu resulting in vomiting and profuse diarrhoea.
“What happens is that sometimes, there is a change in your gut flora, your microbiome and this is typically exacerbated by unnecessary use of antibiotics, which wipe out both good and bad bacteria,” says Dr Yip. “And if you eat a lot of processed foods and don’t have a healthy and well-balanced diet to begin with, meaning prebiotics and probiotics, then you’re setting yourself up for a change in your bowel habits and might now experience IBS symptoms.”

Milestone life events can also trigger IBS. “You see it in people starting their first job, or entering university or the army. All these kinds of things add to the problem,” says Dr Yip, who is seeing IBS in younger patients these days, with the youngest at 16 years of age.
“So your first hit could be that you took a lot of antibiotics to treat a condition. The second hit comes when you don’t have a well-rounded, balanced diet. And then suddenly a milestone in your life happens. That could be the final domino that brings you down.”
And it is precisely this complex interaction between the brain, nervous system, emotions, gut microbiome and gut physiology that makes the disorder so nebulous.
Taking back control
Given that the gut microbiome plays a big part in IBS, it is obviously something to pay attention to. Yet, the ratio between good and bad microorganisms changes with age, as well as one’s diet, stress level and how one’s body is treated.
“That’s why there is no magic bullet to addressing IBS and treatment has to be very holistic,” explains Dr Yip. “You have to be very patient, to systematically address all these problems.”
Undoubtedly, diet plays an important role. Sufferers should follow a low FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) diet. FODMAPs refers to a certain class of carbohydrates which are more difficult to digest and cause cramping, bloating, diarrhoea and/or constipation. These include milk and dairy products, food made with large amounts of barley, rye or wheat ingredients, and those high in fructose, such as tropical juices, honey and high fructose corn syrup.

“Conversely, things that are naturally good for the gut include tempeh, kimchi, Japanese fermented soyabean natto, Greek yogurt and coloured vegetables, which are high in polyphenols,” says Dr Yip. Polyphenols are naturally occurring plant-based micronutrients with strong antioxidant and anti-inflammatory properties.
Sufferers can also take evidence-based probiotics.
Sometimes, it can also be as simple as keeping track of the food items that trigger IBS. These include fried and fatty dishes, spicy food such as mala, or even chocolate, tomatoes, onions, lettuce, coffee and alcohol.
Other treatment options for IBS include behavioural therapies such as stress management and mindfulness, as well as medications for diarrhoea, constipation and pain.
When patients are able to slowly identify and eliminate triggers, it can be successfully managed.
“If they stop eating or drinking something and feel much better, they know they have power over their problems. This means that, say, they go to a birthday party and eat cake and ice cream, they know what’s going to happen to them, but it’s a lot better than saying, ‘oh, I have no power over this’. It gives them the sense and semblance of control – and I think that’s a win.”
Decoding Asia newsletter: your guide to navigating Asia in a new global order. Sign up here to get Decoding Asia newsletter. Delivered to your inbox. Free.
Copyright SPH Media. All rights reserved.

